Pre-symptomatic transmission is very real

Published: June 12, 2021
Share on: Twitter / Facebook
Pre-symptomatic transmission is real. But face masks still don’t work.
Because many authorities justified mask mandates with pre-symptomatic or asymptomatic coronavirus transmission, many skeptics and critics tried to argue against the existence or importance of pre-symptomatic and asymptomatic transmission. But pre- and asymptomatic transmission is real for the same reason that face masks don’t work: aerosols.
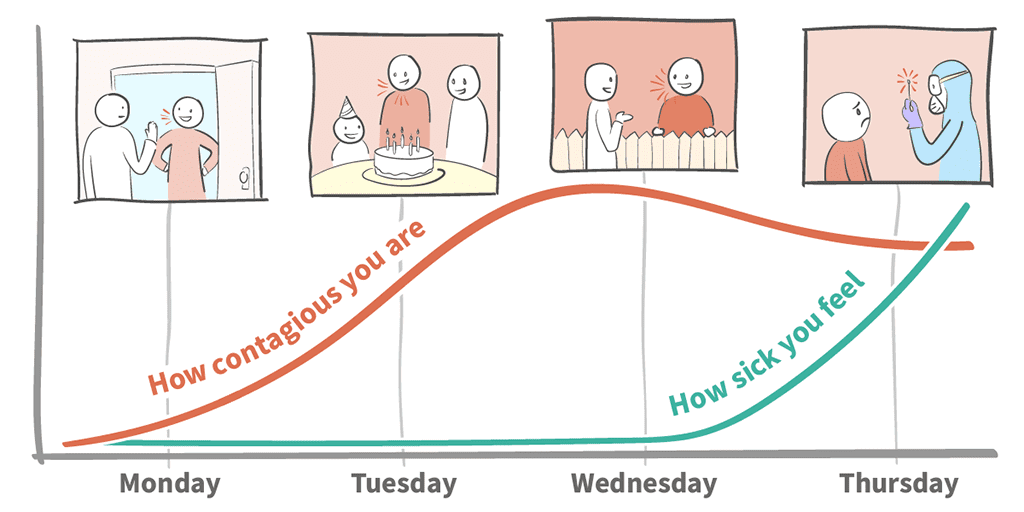
In fact, numerous studies have shown that Sars-CoV-2 respiratory viral load peaks shortly before or shortly after symptom onset (see diagrams below). Once symptoms become apparent, it means the immune system has kicked in and viral load decreases rapidly.
The idea that only symptomatic people spread viral particles, by sneezing or coughing, is based on the obsolete ‘droplet model’ of virus transmission. In reality, transmission occurs primarily, and perhaps almost exclusively, via inhaled aerosols produced when breathing, talking, singing, coughing, or whatever. Droplets, by definition, cannot be inhaled.
Skeptics often point to a famous Wuhan study, published in November 2020 in Nature Communications, that allegedly showed that asymptomatic transmission is a myth, as even a commentary in the BMJ argued. In reality, the Wuhan study was a post-lockdown PCR study which tested 10 million Wuhan citizens in late May 2020 and found 300 who still had a positive PCR test.
But as the study notes, none of these people had positive virus cultures. Thus, these 300 cases were classic post-infectious high-CT PCR positives, who obviously couldn’t infect anyone anymore. In other words, the famous Wuhan study said nothing at all about pre- and asymptomtic transmission.
(Another common misunderstanding about Wuhan is the idea that the city turned into a major coronavirus hotspot. In reality, antibody seroprevalence in Wuhan was only about 1% to 5% by May 2020. At the same time, New York City had already a seroprevalence of at least 20%.)
Pre-symptomatic transmission is already well known from influenza, and it would have been truly surprising if it had played no role at all in the case of the new coronavirus. Indeed, it looks like pre-symptomatic transmission is even more important in the case of the new coronavirus, with estimates ranging between 30% and 60% of all virus transmission.
Pre-symptomatic or “stealth” transmission is also a major reason why Sars-Cov-2 could spread so rapidly and create a global pandemic. The real ‘myth’, or rather exception, might be sick people coughing straight into the faces of healthy people.
In contrast to transmission by pre-symptomatic people (i.e. a few days or hours before symptom onset), transmission by people who remain fully asymptomatic is a bit more complex to evaluate, because this group includes some people with a low viral load, which makes them less contagious. In addition, fully asymptomatic people are much more difficult to detect. However, nobody knows beforehand if they will develop symptoms or not, and as a Swedish doctor recently showed, even fully asymptomatic transmission has been documented in several carefully designed studies.
In conclusion, pre-symptomatic aerosol transmission is very real and has played an important role in driving the coronavirus pandemic. For the very same reason, face masks, ‘temperature screening’, reactive lockdowns, and even ‘contact tracing’ (beyond the very early phase) have not worked.
Postscript
“The abundance of this speech-generated aerosol, combined with its high viral load in pre- and asymptomatic individuals, strongly implicates airborne transmission of SARS-CoV-2 through speech as the primary contributor to its rapid spread.” (‘Breathing, speaking, coughing or sneezing: What drives transmission of SARS-CoV-2?’, Stadnytskyi et al, JIM, June 2021)
Postscript II
The Australian coronavirus outbreak in June 2021 confirmed the key role played by pre-symptomatic aerosol transmission: in a major Sydney cluster, a pre-symptomatic person infected an entire birthday party of 24 people; a pre-symptomatically infected flight attendant went on five domestic flights before testing positive; and an infected nurse traveled for 10 days before testing positive, having already infected several of her contacts.
Postscript III
Even in hospitals, pre-symptomatic aerosol transmission may drive outbreaks: “In this context, our cases consolidated the importance of presymptomatic transmission in the nosocomial outbreak, suggesting that the contact tracing period should be as early as 4 to 5 days before symptom onset.” (Jung et al, ICJ, June 2021)
Scientific diagrams
A) Viral load and culture probability over time
Rapidly decreasing viral load and (especially) infectiousness.

B) Symptom onset compared to peak viral load
Mean delay between peak viral load and self-reported symptom onset is 4 days.

C) Temporal pattern of viral shedding
Rapidly decreasing viral load (PCR ct value) after symptom onset.

D) SARS-1, SARS-2, MERS: Viral load vs. symptom onset
SARS-2: Peak viral load near symptom onset – easy transmission. SARS-1 and MERS: Viral load increases only after symptom onset – poor transmission.

E) Aerosols: Respiratory pathogen transmission routes (2018)
Aerosols as the primary mode of transmission, even at close range.

See also







